Bacterial Armor: The Germs that Become Tanks and How to Eradicate Them

 Eradicating pathogens from environmental surfaces in hospitals is a daily fight. Keeping bacteria from reproducing on surfaces, finding reservoirs in hard-to-clean areas, and forming biofilms requires daily disinfection, and ideally, some form of continuous mitigation. In today's post, we will look at the threats posed by bacteria that are even more adept at surviving on surfaces: Spore-forming bacteria, and how hospitals are trying to keep these persistent pathogens from threatening their patients.
Eradicating pathogens from environmental surfaces in hospitals is a daily fight. Keeping bacteria from reproducing on surfaces, finding reservoirs in hard-to-clean areas, and forming biofilms requires daily disinfection, and ideally, some form of continuous mitigation. In today's post, we will look at the threats posed by bacteria that are even more adept at surviving on surfaces: Spore-forming bacteria, and how hospitals are trying to keep these persistent pathogens from threatening their patients.
| Why "spore"? Typically, the term spore is used to describe a seed-like unit of an organism that reproduces asexually. In bacteria, the spore is actually the cell itself, just in a dormant phase. For this reason, these bacterial cells are more accurately referred to as "endospores." |
Anyone who works in healthcare is well aware that bacteria can survive for a very long time outside of a host organism. Bacteria may cause numerous infections - from minor inconveniences to life-threatening conditions - but they are essentially independent organisms that evolved to live in soil and water, on plant and animal life, and even at the mouths of underwater geysers. They do not require a host to survive. However, some bacteria evolved to become hardier when environmental conditions were not ideal. These bacteria evolved to have a spore life stage, to essentially form a hard shell until environmental conditions became more favorable.
What are the bacteria that survive using a spore developmental state?
Bacillus Species | These Gram-positive facultative aerobes evolved to live in soil. Members of this species are responsible for anthrax in mammals and some strains of food poisoning. Spores that reach an opening in the skin result in what is called a cutaneous infection, while those that are ingested lead to a gastrointestinal infection. Inhaled spores can lead to respiratory infections. Typically, Bacillus initiates sporulation when nutrients are limited, in this case, sugars.
Clostridium Species | These Gram-positive obligate anaerobes are very sensitive to oxygen. When the vegetative forms of Clostridium are deprived of oxygen, they initiate the sporulation process. These spores are the second-most common source of food poisoning. If the spores infect a wound, they will deprive the tissue of oxygen, leading to gangrene. Most alarmingly, Clostridium difficile infections are the number one cause of hospital-acquired diarrhea, and are a particular threat to those undergoing antibiotic treatments (due to resistance). Clostridium species are also opportunistic, meaning they will fill a niche left when helpful gut bacteria are killed by antibiotics. This species is particularly dangerous because it can complete the entire vegetative - spore - regermination - vegetative cycle within the host (unlike Bacillus).
How do hospitals destroy bacterial spores?
Hospitals confront Clostridium far more often than Bacillus, but must have tools to destroy either depending on need.
Bacillus causes hospital-associated infections of wounds and indwelling devices, most notably by the Bacillus cereus bacterium. Studies have found B. cereus to be a high risk for cross-contamination, that is, carried from one patient or surfaces to another patient or surface. These infections can cause septicemia, endophthalmitis, pneumonia, endocarditis, meningitis, and encephalitis, with greatest risk to immunocompromised and/or neonatal patients. Spores have been recovered from patients and surfaces for up to 2 years following an infection. Bacillus spores are extremely resistant to chemical disinfectants, but bleach, with longer contact time, is the best choice.
Clostridium difficile infects over 500,000 Americans each year, of whom 15,000 died due to the infection within a month of diagnosis. While for decades these infections (called CDI) were seen mostly in patients who had received antibiotic treatment and were immuno-compromised, cases are growing among those without these characteristics, as the bacteria adapts to become more virulent. Clostridium spores can live for years on dry, inanimate surfaces such as overbed tables, bed rails, and IV poles. The Centers for Disease Control and Prevention (CDC) recommends the use of an EPA-registered product to kill Clostridium spores, with bleach again a solid choice.
Why are spore-forming bacteria so dangerous in hospitals?
Even though we know what kills spore-forming bacteria, that doesn't mean that our cleaning methods are killing them all each time a surface is wiped down. Because they have evolved to survive, spores can hunker down in crevices, on the undersides of tables, and along rounded surfaces that are not adequately disinfected. Additionally, newer methods of patient room cleaning such as UV radiation and misting don't reach all areas, especially those out of direct line of the dispenser. This is why rigorous, manual cleaning will always be required, but new innovations will be necessary to keep the surfaces clean between disinfection opportunities.
What innovations are successful at killing bacterial spores?
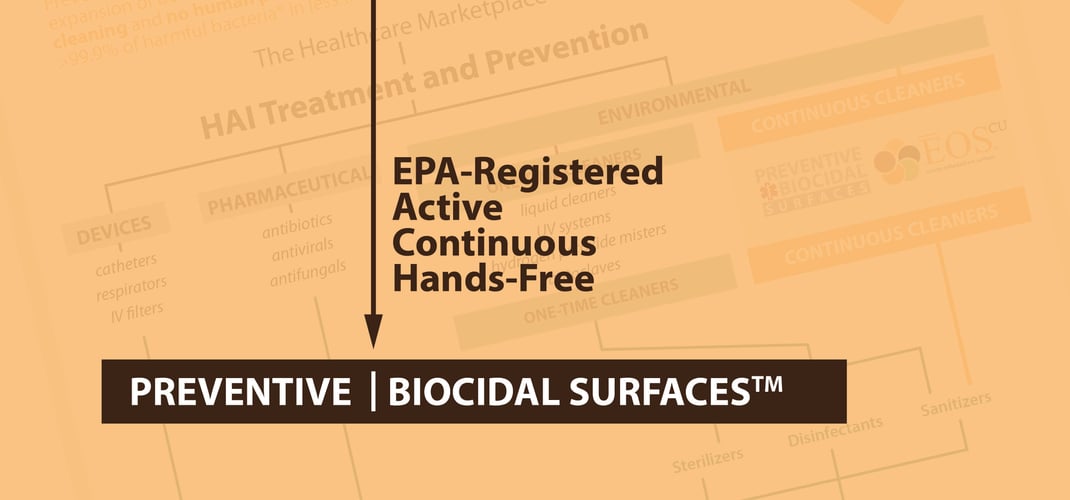
New chemical disinfectants are being registered by the EPA on a regular basis. However, these chemicals can fail due to human error such as incorrect wait times, inaccurate dilutions, missed surfaces, and more. What we need is something that will kill bacterial spores continuously, all day long, even in hard-to reach, overlooked, or ineffectively cleaned areas. One solution is the use of biocidal materials that are non-toxic to us but lethal to both vegetative and sporulated bacteria. The only EPA-registered biocidal material with demonstrated efficacy against spores is copper, which can be found in both alloys and copper-infused EOScu, a synthetic stone surface. By installing these materials on the most-touched surfaces around a patient, the hardest-to-kill pathogens, those that have evolved to evade, can't survive long enough to reach a vulnerable patient.
![EOScu Logo - Dark - Outlined [07182023]-01](https://blog.eoscu.com/hubfs/Eoscu_June2024/Images/EOScu%20Logo%20-%20Dark%20-%20Outlined%20%5B07182023%5D-01.svg)