The Downsides of Contact Precautions
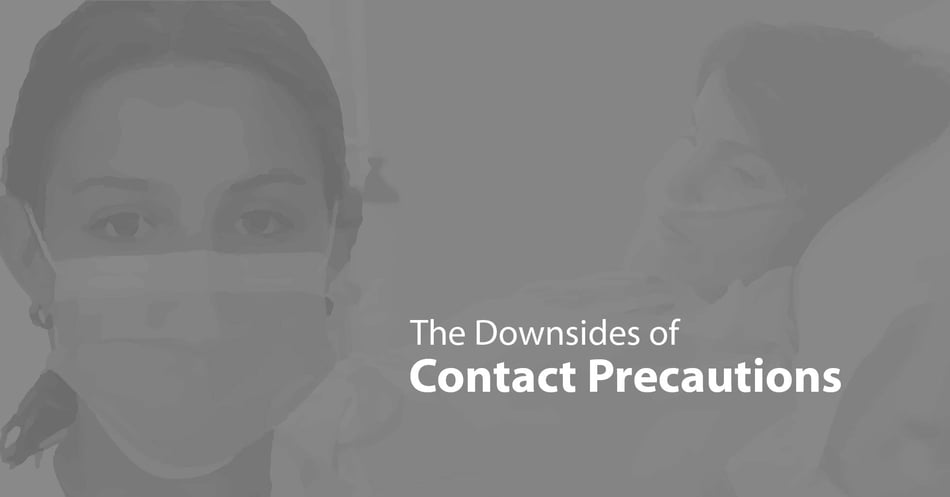
Ever since we first realized that disease could spread through physical contact, medical workers have used barriers to reduce the transmission of germs. Today, the use of gloves, gowns, caps, and other personal protective equipment is the standard for invasive procedures, but it is also used for everyday contact with patients who require isolation. Patients may be put under contact precautions for two reasons: Either to prevent pathogens from entering the room or to prevent pathogens from leaving the room. If a patient is especially vulnerable to pathogens, he or she would need to be protected from pathogens entering the room. The second reason contact precautions are used is when a patient is colonized or infected with a multi-drug resistant organism such as MRSA, VRE, or CRE. In these cases, contact precautions are implemented to prevent pathogens from leaving the room in an effort to protect all the other patients in the hospital. This use of contact precautions is more controversial because the evidence for how effective contact precautions are to reducing transmission is mixed, thereby providing enough doubt as to open the discussion up to consider the downsides of contact precautions.
Medical
Patients face unique medical challenges when placed under contact precautions. Studies show that patients placed under contact precautions in the emergency room take on average 1 hour longer to be transferred to an inpatient room. Once admitted, these patients face further delays in getting diagnostic testing such as radiological imaging and are visited between 20-30% less by health care workers. Those visits tend to be shorter, and more often result in incomplete records. A patient under contact precautions will take almost 2 days longer to place and transfer into a long-term care facility.
Psychological
It is not difficult to imagine the psychological burden of being under contact precautions from the patient's point of view - long delays, fewer visits, and interacting with care givers and loved ones who are covered in masks, gowns, and gloves. It is not a surprise, therefore, that these patients report lower satisfaction scores after their hospital stay. More importantly, studies show that patients under contact precautions have significantly higher rates of depression (40% higher) and delirium (100% higher) - even after accounting for illness, age, gender, and length of hospitalization.
Financial
Healthcare facilities must also consider the financial burden of contact precautions when weighing their costs and benefits. Contact precautions require supplies in caps, gowns, gloves, masks and other personal protective equipment as well as the storage and display space for those items. Donning these items requires time for the healthcare worker entering and exiting the room, but also in reminding and assisting visitors as they learn to follow the requirements. All the garments must also be properly handled in the patient area, as well as once they are bagged and taken out of the hospital for disposal, since they are potentially contaminated materials. Studies also show that the use of contact precautions reduces throughput of patients - the movement of patients through treatment to discharge - reducing the number of available beds for waiting patients and affecting the facilities income.
Adherence and Impact
All these costs may seem manageable if they work. Unfortunately, as more patients are treated with contact precautions, the rates of adherence go down. After about 60% of patients are under contact precautions, the more likely a health care worker is to skip the protocol. Added to that fact is that even when the protocols are followed, there is scant evidence to show that contact precautions prevent transmission of MDROs. For the amount of time they take to implement properly, the resulting reductions are minimal: Out of hundreds of patients under contact precautions, only 1 MRSA acquisition would be prevented, and even that one acquisition has only a 33% of becoming an infection.
The Controversy
There will always be a place for careful isolation of some patients, but current discussions are moving in the direction of stopping the wholesale use of contact precautions for many patients. Pathogens are still moving throughout a hospital despite the use of contact precautions, so other options must be explored. Controlling the colonized or infected patient's environment is key in this effort. Decolonization of the patient through the use of bathing or nasal swabs can control the patient's biome, while using materials around the patient that actively reduce the bioburden can control the environment. These methods reduce the change of transmission without some of the costs associated with contact precautions.
![EOScu Logo - Dark - Outlined [07182023]-01](https://blog.eoscu.com/hubfs/Eoscu_June2024/Images/EOScu%20Logo%20-%20Dark%20-%20Outlined%20%5B07182023%5D-01.svg)

![[INFOGRAPHIC] Anatomy of an Isolation Room](https://no-cache.hubspot.com/cta/default/216314/interactive-178534055548.png)