Isolation Rooms: Types and Challenges
Thanks to the COVID-19 pandemic, we are all very aware of the need for isolation in a hospital. But did you know there are different types of isolation rooms, each with its own unique purpose? These specialized rooms are designed to protect people - patients, staff, and visitors - by controlling the spread of pathogens, each in its own way. Let’s dive into the main types and what makes each one important!
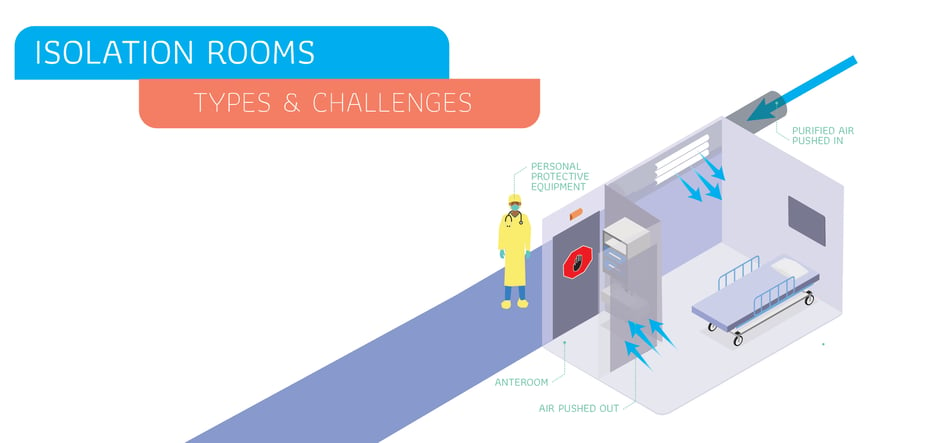
1. Negative Pressure Rooms/AIIRs: Keeping Contaminants In
Negative pressure rooms, now called airborne infection isolation rooms (AIIRs) are designed to keep harmful pathogens from leaving the room. These rooms are especially important for patients with contagious respiratory illnesses like tuberculosis, COVID-19, measles or influenza, where the pathogens are airborne. The "negative pressure" means that air in the room is at a lower pressure than the areas outside the room, so every time the door is opened, air is pulled into the room. This flow prevents contaminated air from escaping into other areas of the hospital. The contaminated air is filtered and exhausted outside or through specialized systems, ensuring that harmful particles are removed safely. These are considered Class N Isolation Rooms or in the case of a highly dangerous pathogen, a Class Q (Quarantine) Isolation Room.
2. Positive Pressure Rooms: Keeping Contaminants Out
On the flip side, positive pressure rooms do the exact opposite! These rooms are for patients who need protection from the outside environment, such as those undergoing chemotherapy, transplant patients, or anyone with a compromised immune system. In a positive pressure room, clean, filtered air is constantly pushed into the room, keeping it at a higher pressure than the surrounding areas. Each time the door is opened, the air flows out of the room, preventing any unfiltered air from entering. This flow keeps harmful bacteria or viruses away from vulnerable patients, giving them the best chance to recover without exposure to outside contaminants.
3. Protective Isolation Rooms: Keeping Vulnerable Patients Safe
These rooms are similar to positive pressure rooms but have a heightened focus on keeping immunocompromised patients safe from any type of infection, not just airborne contaminants. They might have special filtration systems or other features like anterooms (a small entry space between the main hospital area and the isolation room) where staff can put on protective gear before entering. The goal is to create a bubble of safety around the patient, ensuring they are exposed to as few pathogens as possible. These rooms are typically used in oncology, burn units, and neonatal units. These are called Class P Isolation Rooms.
4. Contact Isolation Rooms: Minimizing Surface Contamination
Contact isolation rooms are designed for patients with infections that spread through direct contact with surfaces or skin-to-skin contact. Infections such as MRSA (Methicillin-resistant Staphylococcus aureus) or C. difficile require these precautions. Healthcare staff and visitors entering these rooms wear protective gowns and gloves (PPE) to prevent picking up germs from surfaces and spreading them to other areas. These rooms do not need special air flow equipment or seals; any room can become a contact isolation room depending on need just by requiring all who enter to don PPE. They are Class S Isolation Rooms.
5. Droplet Isolation Rooms: Blocking the Spray of Germs
Ever sneeze and see tiny droplets in the air? That’s how some infections, like the flu or pertussis, can spread. Droplet isolation rooms are designed for patients with illnesses that travel in these droplets. To prevent germs from spreading when patients cough, sneeze, or talk, hospital staff will often wear masks when entering these rooms. Like contact isolation rooms, they don't require special equipment and are designated as such based on patient needs. They are also Class S Isolation Rooms.
Challenges for Infection Control and Prevention
Isolation rooms are not the answer to every infection situation - just one of many necessary tools. Protecting patients from infection is problem with many "heads," much like the mythological creature Hydra. We must attack all the heads at once to make a difference. To fight antibiotic resistance, we must use antibiotic stewardship. To fight insufficient terminal cleaning, we must emphasize checklists, preventive biocidal surfaces, and a culture of improvement. To address device-associated infections, we need a system-wide approach to lowering device days along with safety checklists and protocols. And none of these efforts will be enough if staff shortages or cost cutting place too much responsibility on too few people, however dedicated and proficient those people may be. Investment in technologies (such as EPA-registered copper-infused biocidal surfaces) that provide a safety net is a cost-effective way to reduce hospital associated infections - inside and outside of isolation rooms - while we attack all those problems head-on.
What are your experiences with isolation rooms, both as a patient and as a caregiver? Share your thoughts in the comments below!
![EOScu Logo - Dark - Outlined [07182023]-01](https://blog.eoscu.com/hubfs/Eoscu_June2024/Images/EOScu%20Logo%20-%20Dark%20-%20Outlined%20%5B07182023%5D-01.svg)

![[infographic] Types of Isolation Rooms Download and share!](https://no-cache.hubspot.com/cta/default/216314/interactive-181620705846.png)